If you’ve ever worked in or around a hospital, you’ve probably heard the term EHS mentioned in safety meetings or compliance training. It stands for Environmental Health and Safety, a system that keeps healthcare settings safe, healthy, and compliant. In simple terms, EHS is about preventing harm before it happens. It ensures doctors, nurses, technicians, and even patients can focus on care without worrying about chemical exposure, infections, or workplace hazards. Understanding what EHS means in medical terms helps explain how hospitals and clinics protect people and the environment every single day.
Understanding EHS in a Medical Context
In healthcare, every decision has a ripple effect. From how waste is handled to how workers are protected from infection, small actions can make a big difference in safety and outcomes. That’s where EHS comes in.
EHS stands for Environmental Health and Safety. It’s the framework hospitals, labs, and clinics use to protect people, maintain compliance, and minimize environmental harm. The concept may sound administrative, but in reality, it touches almost everything in a medical facility. It’s the reason staff wear protective gear, patients aren’t exposed to biohazards, and waste doesn’t contaminate the environment.
EHS isn’t a single policy or checklist. It’s an ongoing system that integrates environmental protection, occupational health, and workplace safety. In medical terms, EHS acts as the invisible backbone of hospital operations, keeping both people and the planet safe.
The Three Core Pillars of EHS
Although EHS appears as one term, it actually combines three interdependent pillars that work together.
1. Environment
Environmental protection focuses on preventing pollution and waste within healthcare operations. Hospitals generate medical waste, chemicals, and emissions that can harm ecosystems if mismanaged. EHS standards help manage everything from water use and air quality to hazardous materials storage.
2. Health
Occupational and public health are central to EHS. The goal is to prevent disease, protect staff from occupational hazards, and ensure that the facility itself doesn’t pose health risks. This includes infection control, vaccination programs, ergonomic assessments, and employee wellness initiatives.
3. Safety
The safety component ensures that staff and patients are physically protected. It covers training, emergency preparedness, personal protective equipment (PPE), radiation safety, and response plans for incidents.
Together, these pillars create a structured approach to running healthcare facilities responsibly and safely.
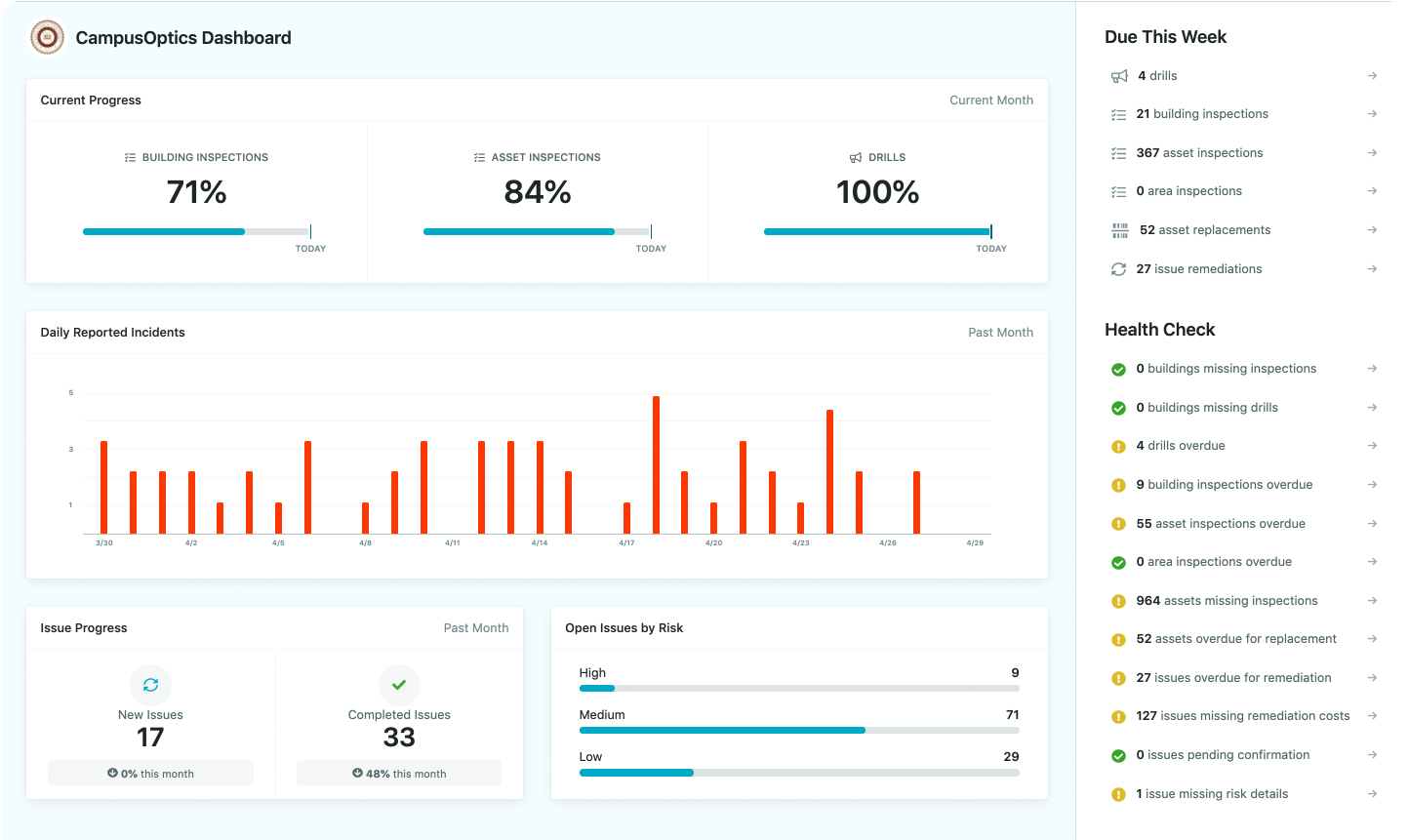
How We Support EHS Through CampusOptics
At CampusOptics, we’ve seen firsthand how complex EHS management can be, especially in environments where safety, compliance, and collaboration all overlap. Our platform was designed to make those challenges simpler, helping organizations stay organized, compliant, and connected.
We built CampusOptics to give Environmental Health and Safety professionals a clear, accessible way to manage the moving parts of safety operations. Through one comprehensive system, teams can track chemical inventories, log incidents, manage inspections, and monitor compliance deadlines without juggling separate spreadsheets or disconnected tools.
What makes this work in real life is usability. EHS professionals are rarely sitting behind a desk, so our mobile tools allow quick access to safety data, reports, and emergency plans from anywhere on campus or within a facility. Features like barcode scanning, talk-to-text entries, and in-app photo uploads make fieldwork faster and more accurate.
We also believe that a strong safety culture starts with visibility. That’s why our platform helps map safety assets, monitor risk trends, and generate reports that turn complex data into clear insights. By connecting every department: from environmental safety to fire and life safety, we help institutions improve collaboration, reduce risk, and maintain the confidence that their EHS program is built to last.
Benefits of Implementing EHS Programs in Healthcare
Hospitals that invest in structured EHS programs see measurable improvements across safety, efficiency, and morale.
Here are the most common benefits:
- Fewer accidents and injuries: Proactive hazard identification prevents harm before it occurs.
- Better infection control: Structured hygiene and sterilization protocols reduce hospital-acquired infections.
- Lower legal and financial risk: Compliance minimizes fines and liability claims.
- Improved staff retention: Workers feel safer and more valued.
- Enhanced reputation: Safety and sustainability attract patients and employees alike.
- Cost savings: Reduced waste, lower energy bills, and fewer lost workdays translate into long-term financial benefits.
An effective EHS program doesn’t just prevent disasters; it makes the entire organization run smoother.
Why EHS Matters in Healthcare
Hospitals and clinics are complex environments. Doctors, nurses, and technicians handle biological agents, chemicals, and heavy machinery every day. Without strong EHS systems, the risk of injury, contamination, or environmental harm rises quickly.
Here’s why EHS is so crucial in medical settings:
- Patient safety: Prevents cross-contamination and infection through sterilization, air filtration, and safe disposal of medical waste.
- Worker protection: Reduces injuries, radiation exposure, and chemical contact.
- Regulatory compliance: Ensures facilities meet local and international safety laws, including OSHA and EPA regulations.
- Environmental responsibility: Helps hospitals minimize pollution, conserve energy, and manage resources sustainably.
- Operational efficiency: Reduces downtime from incidents or non-compliance penalties.
Ultimately, EHS isn’t just a compliance box to tick, it’s a philosophy of prevention. When done right, it supports a culture of care that extends from patients to the wider community.
The Role of EHS Professionals in Healthcare
Behind every safe healthcare environment is an EHS team that works quietly but relentlessly. EHS professionals design and monitor safety systems, train staff, and ensure that the facility meets both internal and external standards.
Their responsibilities include:
- Conducting risk assessments to identify hazards.
- Overseeing waste management and disposal.
- Managing chemical inventories and safety data sheets.
- Coordinating emergency response plans.
- Ensuring regulatory reporting and audit readiness.
- Promoting sustainability initiatives like recycling or energy conservation.
In healthcare, these roles often overlap with infection control officers, quality assurance teams, and facility managers. Together, they create a safety network that supports daily operations.
EHS and Sustainability in Modern Healthcare
Modern hospitals are not just medical centers; they’re large ecosystems that consume significant amounts of energy, water, and materials. Integrating EHS with sustainability goals helps these facilities reduce their environmental footprint while maintaining patient safety and operational efficiency.
In practice, this means building systems that manage waste responsibly, conserve resources, and choose environmentally conscious suppliers. Hospitals are adopting recycling and waste segregation programs, monitoring their energy and water use, and improving air quality inside and outside their buildings. Many also invest in eco-friendly procurement practices and sustainable infrastructure, designing greener buildings that support long-term efficiency.
These efforts go beyond environmental compliance. They help hospitals save money, streamline operations, and build public trust. More patients today care about sustainability, and hospitals that actively reduce their impact often find that environmental responsibility complements their reputation for quality care.
How to Strengthen EHS in a Healthcare Setting
Building an effective EHS program takes strategy, commitment, and collaboration. It’s not something you can implement overnight; it grows with consistent effort and leadership support. Below are practical ways healthcare organizations can make EHS work in real life.
1. Start With a Thorough Risk Assessment
The first step is understanding where your vulnerabilities lie. Identify areas where hazards are most likely to occur: labs, waste zones, operating rooms, and chemical storage areas are common hotspots. Evaluate everything from biological risks to physical safety hazards. A detailed risk map helps you prioritize what needs attention first instead of trying to fix everything at once.
2. Develop Clear, Realistic Policies
Policies are the foundation of an EHS program, but they only work if they’re specific and easy to follow. Document procedures for chemical handling, waste disposal, emergency response, and infection control. Make sure these policies are accessible and reviewed regularly to stay in line with new regulations or technologies.
3. Train Consistently and Practically
Safety training shouldn’t be a checkbox exercise. It has to be continuous and relevant to daily work. Regular refreshers keep staff aware and confident, especially in high-risk areas. Use short, practical sessions, simulation drills, and peer-to-peer learning to make training stick instead of relying solely on formal lectures.
4. Use Technology to Simplify Compliance
Adopting EHS software can make a huge difference. Digital tools help track incidents, manage audits, and generate compliance reports in real time. Mobile apps also make it easier for healthcare workers to log safety issues or complete inspections on the go, reducing delays and paperwork. Technology doesn’t replace human oversight, it enhances it by keeping data organized and actionable.
5. Foster a Culture of Safety and Trust
The best safety programs don’t rely on enforcement alone; they thrive on openness. Encourage staff to speak up about near misses, unsafe conditions, or potential hazards without fear of blame. Recognize those who take initiative. When people feel heard and supported, they’re more likely to take ownership of safety rather than see it as someone else’s job.
6. Monitor and Measure Performance
An EHS program is never “finished.” Regular audits, inspections, and data analysis help spot gaps early. Review trends in incident reports, training completion, and environmental impact. Share findings transparently so teams can see progress and understand why adjustments are made.
At the end of the day, an EHS system only works when everyone, from janitors to surgeons, understands their role in maintaining safety. It’s a collective effort that blends policies, technology, and human behavior into one shared mission: keeping healthcare environments safe, healthy, and sustainable.
The Future of EHS in Medicine
EHS is evolving alongside healthcare itself. New challenges like antimicrobial resistance, digital record management, and climate change are reshaping how hospitals think about safety and responsibility. The next phase of EHS will rely heavily on technology, data, and behavioral insight to build stronger, more adaptive systems.
Artificial intelligence is already being used to predict incidents and identify risk patterns before they lead to harm. Mobile tools make it easier for healthcare workers to collect safety data in real time, directly from the field. Hospitals are also moving toward sustainable designs that prioritize low emissions, energy efficiency, and eco-friendly materials.
At the same time, integration between EHS, HR, and clinical data systems is helping organizations make faster, evidence-based decisions. Many are also focusing on behavioral safety programs that strengthen leadership engagement and encourage a culture of accountability.
The future of EHS isn’t just about compliance anymore, it’s about using technology, collaboration, and foresight to make healthcare more resilient, sustainable, and human-centered.
Final Thoughts
EHS might not be the most visible part of healthcare, but it’s one of the most important. It’s what keeps hospitals running safely, quietly preventing harm while supporting every aspect of patient care. In medical terms, EHS is more than just an acronym, it’s a promise to protect people, preserve the planet, and maintain trust in the places where health begins.
FAQs
What does EHS stand for in medical terms?
EHS stands for Environmental Health and Safety. It’s a framework used in healthcare to protect patients, staff, and the environment from potential risks. It includes everything from infection control and waste management to workplace safety and compliance with regulations.
Why is EHS important in healthcare?
EHS ensures hospitals and clinics maintain a safe environment for both workers and patients. It prevents injuries, reduces infections, minimizes environmental damage, and helps healthcare facilities stay compliant with safety and environmental laws.
Who is responsible for EHS in a hospital?
EHS is a shared responsibility, but most hospitals have dedicated EHS professionals or teams. They conduct risk assessments, oversee safety programs, train staff, and ensure compliance. Every employee, from doctors to maintenance staff, also plays a role in maintaining safety.
How does EHS help protect patients?
EHS policies help reduce the spread of infections, manage hazardous materials safely, and ensure equipment and facilities meet health standards. This results in safer environments and better outcomes for patients.
What are some examples of EHS programs in healthcare?
Common examples include infection prevention plans, emergency preparedness drills, waste disposal systems, radiation safety protocols, ergonomic assessments, and sustainability initiatives like energy conservation and recycling.